STAT stories
STAT has been successfully implemented by service providers across Australia and New Zealand. Learn more about some of the places the STAT has been implemented, or get in touch with our team to share.
Application to paediatric community health services
Community based therapy services for children, such as speech and language therapy, occupational therapy and physiotherapy are often faced with high demand and long waiting lists. The consequences of waiting for these services can be significant, as children miss out on an important window of opportunity for treatment as their young brains develop and they move through educational milestones such as starting school.
The CSTAT project trialled the STAT model in 5 paediatric community health services in Melbourne. The project was funded by the Department of Health and Community Services, as well as the Medical Research Future Fund (MRFF) via funding for a Translating Research Into Practice Fellowship held by Principal Investigator Dr Katherine Harding.
The results of this study were presented as a poster at the biannual conference of the Health Services Research Association of Australia and New Zealand in, Sydney, December 2022.

Application of STAT to an outpatient medical clinic
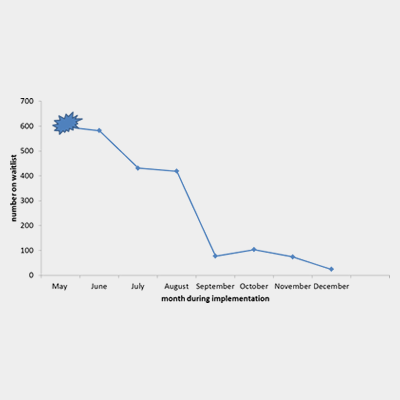
Annie Lewis led the first trial of the STAT model in a medical outpatient clinic. This before and after trial with a time series analysis and process evaluation was set in the epilepsy clinic at Box Hill Hospital. A waitlist of 600 people was virtually eliminated through a structured backlog reduction approach, without increasing the waiting time. A poster describing the backlog reduction process was delivered by Annie at the Epilepsy Society of Australia Annual Conference, and awarded a special commendation by the Education and Scientific Meeting Committees in recognition of an outstanding scientific presentation.
A follow up of the clinic two years after STAT was implemented showed that benefits had largely been sustained, although there were some early signs of old habits returning. This study highlighted a range of issues that need attention to ensure long term sustainability of wait list interventions.
WaitLESS: Innovative research funded to reduce wait times for specialist medical care
Congratulations to Prof. Katherine Harding for leading an application to successfully securing $1.46 million in funding as part of the National Health and Medical Research Council (NHMRC) Partnership Project scheme.
In conjunction with the Eastern Health Institute, this project will run trials in eight outpatient medical clinics across the Eastern Health network, implementing the STAT model to establish a process for reducing wait lists that can be replicated elsewhere.
Find out more about the National Health and Medical Research Council (NHMRC) Partnership Project scheme.

Community Health Demand Management Toolkit
After a long consultation process with researchers, service providers and other key stakeholders, the Department of Health released a new Demand Management Toolkit for Community Health in May 2023. This document replaces the previous Demand Management Framework for these settings. An outdated focus on triage tools to guide access to services has now been replaced with an approach more consistent with principles of the STAT model: understanding supply and demand, streamlined access, early assessment, and delivery of services in a way that considers capacity and patient flow. The STAT team at Eastern Health / La Trobe University is excited to be partnering with Department of Health during 2024 to support the implementation of the new toolkit in community health services across Victoria.

Implementation of STAT at Illawarra Shoalhaven LHD
Workplace: Illawarra Shoalhaven Local Health District – NSW Health
Zoe Fitzgerald is a Senior Clinical Neuropsychologist and the Psychology Unit Head at Illawarra Shoalhaven Local Health District of NSW Health. Zoe has generously agreed to share her story with us and the STAT community.
Zoe works in an outpatient Neuropsychology and Psychology service in the vast Illawarra Shoalhaven Local Health District. Due to the high cost of private assessments their Neuropsychology service, the sole provider in the health district, faces significant demand.
For over 13 years, the service struggled with demand management, consistently there was a 12-18 month wait for Neuropsychology. While they implemented various waitlist management projects they had little success. Sadly, it was not uncommon to learn of client’s health deteriorating or even passing away when finally reaching out to offer appointments. These long wait times clearly were not providing the timely care this population needed. This reality weighed heavily on Zoe and her colleagues. As they phrase it, “we were always burdened by the waitlist”.
The clinicians in the unit enjoy seeing clients and providing timely, meaningful & gold standard clinical care, this has always been how they define success. However, the waitlist created pressure to rush through tasks, leaving them feeling as though they were moving away from their gold standard of clinical care. In turn, this fueled feelings of guilt, as they felt prevented from delivering the quality of care they valued.
In registering for the STAT workshop Zoe thought “we’ve got nothing to lose”. After attending, Zoe was optimistic but thought, this is great… but how can this work in our service and model of care. The main barriers identified to implementing STAT were; lengthy assessments and report writing with each client, limited EFT and limited funding/staff to clear the backlog.
Zoe’s team calculated demand based on STAT principles and as well considered the EFT hours on average required for each client. However, the backlog remained a significant barrier.
In this context, the COVID-19 restrictions turned out to be a blessing! Unable to see clients face-to-face and the limited ability to conduct neuropsychology assessments virtually, clinicians turned their attention to the waitlist. They were able to conduct clinical triage calls with the entire waitlist and found, not everyone needed a full battery of tests, instead clinicians were able to provide alternative assistance such as assessment variations, psychoeducation and redirection to more appropriate service as indicated.
Now, clinical triage calls and dedicated initial appointment slots are routine. Clients are assigned to a clinician and contacted for a triage call within a month of referral, followed by a first visit 1-3 weeks later. This wait time has held steady for 3 years.
STATs impact is widespread. Clients are pleasantly surprised by speedy appointments, and doctors have commented on the efficient follow-up. Surveys show happier clinicians, Zoe says they feel helpful and efficient, which families value, “as a clinician who is there to help people, it’s extremely satisfying”.
Zoe’s key advice for implementing STAT? Make it work for you. Continuously review and adapt based on your specific needs. We’re also thrilled to that Zoe found the STAT team to be a supportive and responsive point of contact for any issues that might arise.
Benefits of a Seating Clinic
Name: Nellie Solano, Senior Occupational Therapist
Workplace: Healesville Hospital & Yarra Valley Health – Eastern Health
Nellie Solano is a Senior Occupational Therapist in Community Health at Healesville Hospital and Yarra Valley Health. With an ageing population in a large geographical area, she reported that the OT team were spending a significant amount of time arranging individual seating/recliner chair trials in clients’ homes. Issues included significant travel time, coordination and communication with multiple stakeholders (equipment supplier, client, family, SWEP), repetitive manual handling for equipment suppliers, and completion of paperwork for funding applications.
Nellie and her team completed STAT training and identified the need for efficient workflow practices to manage demand for OT services. The team came up with the idea of having a monthly chair trial day on site where equipment suppliers attended the Community Health service with numerous chair options that could be trialled by all those referred for seating assessment
The benefits of a seating clinic included:
- Elimination of OT travel time (non-attributable time).
- Increased number of chair trials that could be completed in a much shorter timeframe.
- Providing a timely service.
- Increasing staff and consumer satisfaction.
- KPIs more achievable.
- Reduced communication and coordination required, as everyone knows clinic dates in advance.
- A shared spreadsheet was developed to plan dates with supplier and inform clients on upcoming dates.
- Equipment company scheduled in advance.
- Room booked.
- OTs can book clients straight into next available clinic.
- Client has time to arrange transport.
- AHA delegated with administrative tasks, freeing up OT for other clinical work.
- AHA also trained in ‘white’ prescription so can commence SWEP applications and input basic details.
- Staff able to keep up with recurring STAT assessment blocks.
The seating clinic was implemented in 2020 and has been sustained during that time due to its success.